Palliative Care and End-of-Life Planning
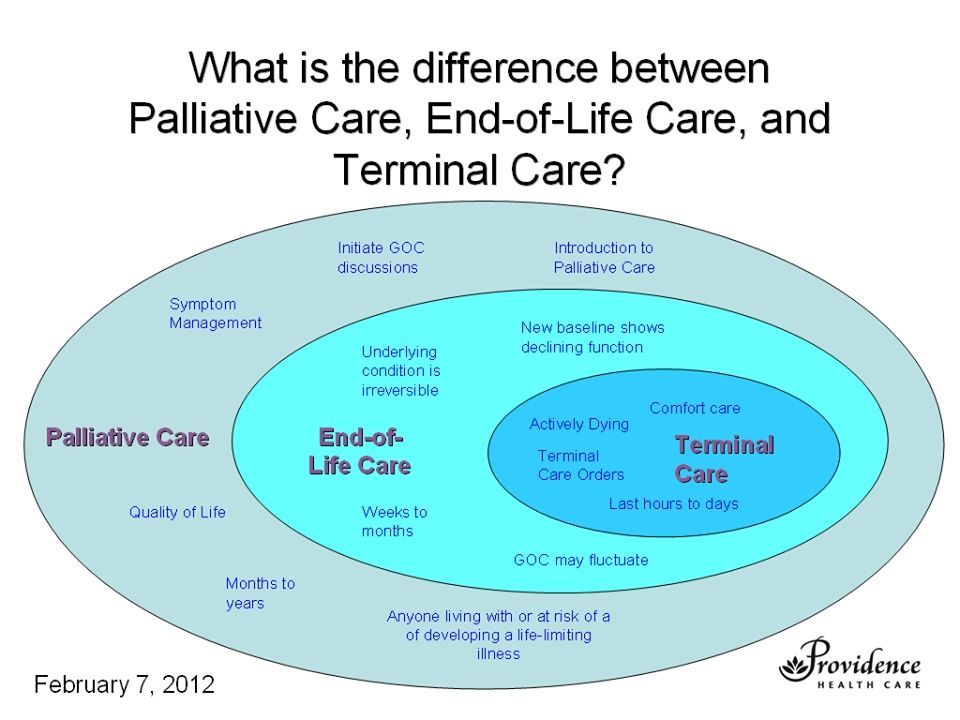
Palliative care is a specialized approach to healthcare that focuses on providing relief from the symptoms and suffering associated with serious illnesses. It aims to improve the quality of life for patients and their families, especially those facing life-threatening conditions. End-of-life planning, on the other hand, involves making decisions about medical treatments and interventions when a person is nearing the end of their life. It helps individuals ensure their preferences and values are respected and followed during this challenging time.
Importance of Palliative Care
Palliative care plays a crucial role in managing the physical, emotional, and psychological symptoms of patients with severe illnesses. It provides a holistic approach to care, focusing not only on treating the disease but also on addressing the person’s overall wellbeing. Palliative care teams consist of healthcare professionals, such as doctors, nurses, and social workers, who work together to develop personalized care plans that are tailored to the patient’s specific needs.
Components of Palliative Care
Palliative care encompasses various components that work in harmony to meet the needs of patients. These include:
Pain and Symptom Management: Palliative care specialists are trained to effectively manage pain and alleviate symptoms, providing comfort and relief.
Emotional and Psychological Support: Patients and their families may experience emotional distress and anxiety. Palliative care offers counseling and support to help individuals cope with these challenges.
Spiritual Care: Recognizing the importance of spiritual beliefs, palliative care teams provide spiritual support to patients and their families.
Coordination of Care: Palliative care professionals collaborate with other healthcare providers to ensure seamless transitions between different stages of care.
Benefits of End-of-Life Planning
End-of-life planning involves making decisions about medical treatments, as well as documenting preferences regarding life-sustaining interventions, funeral arrangements, and distribution of assets. It offers several benefits, including:
Empowerment: Planning for end-of-life allows individuals to have control over their medical care, providing a sense of empowerment and peace of mind.
Relieving Burden: By clearly expressing one’s wishes, end-of-life planning helps relieve the burden on family members and loved ones, who would otherwise have to make difficult decisions on their behalf.
Ensuring Dignity: End-of-life plans help ensure that a person’s desires for their care and treatment are respected, promoting dignity even in the most challenging times.
Reducing Conflict: Planning in advance can minimize conflicts among family members, as everyone is aware of the individual’s wishes and intentions.
Combining Palliative Care with End-of-Life Planning
Both palliative care and end-of-life planning complement each other and should be considered together to provide the best possible outcomes for patients. While palliative care focuses on providing comfort and symptom relief, end-of-life planning ensures that those preferences are appropriately respected when it matters most.
Conclusion
Palliative care and end-of-life planning are integral aspects of healthcare that prioritize the wellbeing, comfort, and dignity of individuals facing serious illnesses. By combining these approaches, patients can receive holistic care while having their preferences and values honored. It is essential for individuals to familiarize themselves with both palliative care and end-of-life planning, empowering them to make informed decisions and find solace in their final stages of life.